A broken healthcare system
Healthcare in Australia and elsewhere, is about creating better health outcomes for patients. There are many elements to the system, and many operators, and whilst each of them has their own specialty functions, together the system is supposed to operate cohesively and with the primary purpose always at the fore. But does it operate that way? The truth is that whilst some elements work very well, others tend to let the team down. There are however solutions or ideas in place to change and improve the less well functioning elements of the system.
One solution for any problem in government has always been to allocate more money to that issue. This may have a political windfall, but Professor Zoe Wainer, the Deputy Secretary for Public Health at the Victorian Department of Health, says that “more money isn’t the solution.” In fact, “there’s no correlation between extra spending and health outcomes.” The problem in Victoria is not funding but the fact that “the health system was never really designed.” It’s a patchwork “without a broader vision.” Essentially, it “evolved to respond to immediate needs, and that is still the system we have today.” Not only is there constant confusion between the private and public health systems, but even in a country with so-called universal healthcare, “there are growing disparities in equity of access to health care and outcomes.” The real goal of any system is to create value, be it societal, economic, environmental or any other kind of value. But in the current health system in Victoria, that is seemingly not possible.
“How can we do that with a system that is structured with very little design or definition?”
Professor Zoe Wainer, Deputy Secretary, Public Health, Department of Health (Vic)
The real issue is that from a systemic perspective, it has always been about “what the doctors say, not what the patients need. For instance, we don’t have chest pain clinics, we have cardiology clinics, though no one ever presents to a doctor with a cardiology problem.” The upshot of that is that doctors and others spend a significant portion of their time “navigating the system for our patients.”
Value-based healthcare
For a system that wasn’t properly designed and doesn’t always work for the benefit of the patients, the only way to disrupt it is by adding value from the ground up, in other words “improving health outcomes that matter to people and populations by investing every precious health dollar in the wisest way possible.” This is a framework called ‘value-based healthcare’, which was coined by the Harvard Business School.[1] In simple terms, it is about “the right care designed around the patient, at the right place, by the right clinician at the right time.” In Victoria at least, that is not how it is currently set up.
The problem in most health systems – which is not necessarily their fault – is that they were set up or came about “to respond to the immediate need.” After all, this is what first aid is all about and why the emergency services exist. Yet at the same time, once a system starts to become developed, it needs a broader reason for being, and in general, “we have not taken a long-term vision about the implications and potentially unwanted implications of that design, or lack of design.” Many medical professionals have identified problems in the system and often try to redress them, but sometimes these piecemeal solutions have “unintended consequences.” Value-based healthcare provides “a set of principles in a framework that actually allow us to redesign the system holistically.”
The principles of value-based healthcare
The concept of value-based healthcare was introduced by Harvard Business School in 2013. At that time they created a model of six principles,[2] which are still relevant today with real-world applications:
- Integrated Practice Units – These are intended to be units of care for the “whole cycle, from prevention, to admission, to care and to palliation.” In other words, “care that’s designed around patients with common clinical needs.” If this were to happen, “our system would look very different.”
- Measure Outcomes and Cost for Every Patient – This refers to outcomes that matter to patients. Currently “we only measure outputs and inputs.” This usually manifests in “the absences of negative outcomes.” The outcome a patient desires is pain relief, not the lack of another appointment.
- Move to Bundled Payments – This goes hand-in-hand with the previous principle. Dental Health Services Victoria as an example, measured the cost of “getting a patient from the door of the Royal Dental Hospital into the dental chair in the emergency department.” The cost was $80 “before a single health outcome has been delivered or even started.” This could be “profoundly changed with investment in different and bundled payment models.”
- Integrate Multi-site Care Delivery Systems – Rather than requiring navigation, “patients actually want the care to be coordinated and for the system to do the work for them.”
- Expand Geographic Reach – “We need multidisciplinary teams responsible for the full care cycle allocated to sites based on a site’s capability.” During the pandemic, some of this virtual care showed that it was possible, but now this needs to be consolidated.
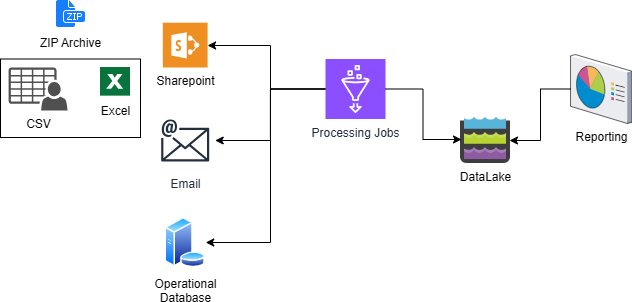
- Build an Integrated IT Platform – “We have digital technology solutions expanding with the real-time sharing of clinical data.”
Most of these principles are somewhat utopian. If the goal is to achieve all of this within the current health system then it clearly won’t happen. “For us, it is really important that that doesn’t stop us, because it could quite easily be a barrier.” What is necessary is to focus on the things that can be achieved and to appreciate that “most of the principles are not new and that many organisations are at some level, already engaged in some of these principles.” Ultimately it is up to the leaders of the health sector to “set the strategy by understanding the intrinsic connection of culture, strategy and measurement. System change comes from being bold and setting those aspirations.”
To get real value from the healthcare system, those in charge need to know what to measure and why, but “this can be an enormous challenge.” Within the framework of value-based healthcare are three indicators to assist with that: capability (a patient’s functional status); comfort (relief from physical and emotional pain); and calm (the extent to which a patient can continue with their lives). This goes one way towards “moving away from just capturing outcomes about an individual disease or condition, and towards actually capturing what matters to people in their lives.” This goes beyond “processes and hospitality” and focusses on “improving the value of treatment.” These measures also come from the patients themselves, which is critical.
In the Victorian health system, “we are shifting our systems to a population health and equity focus, and as much as we can, we are trying to keep our communities well in place.” To do this, “we are not only resilient, but anti-fragile, which means strengthening in the face of shock.” There are more shocks coming, but “our system needs to be strong enough in order to respond in a meaningful way.”