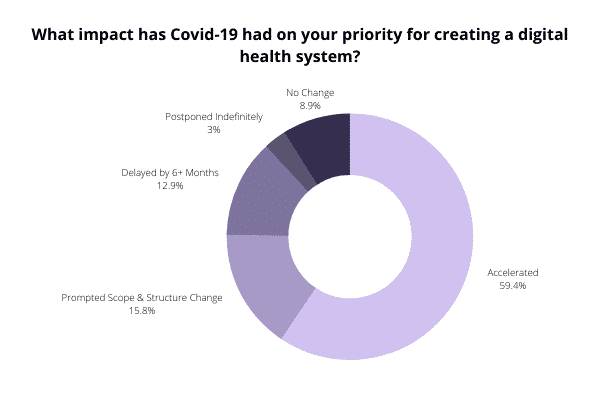
The COVID-19 pandemic is placing enormous strain on the global health care sector’s workforce, infrastructure, and supply chain, and exposing social inequities in health and care. COVID-19 is also accelerating change across the ecosystem and forcing public and private health systems to adapt and innovate in a short period.
The Covid-19 pandemic has, and still is, placing enormous strain on the Australian healthcare sector. Everything from workforce to infrastructure, supply chains and access to care have had a spotlight shone on them in the last 20 months.
While exerting strain and revealing how vulnerable the healthcare industry is, the pandemic has also accelerated change, encouraging – and sometimes forcing – health systems, providers and operators to adapt and innovate digitally in a short period.
Digital transformation in healthcare has always been important, but recently it has become a priority. Technologies like telemedicine, artificial intelligence (AI)-enabled medical devices, and shared electronic medical records are just a few concrete examples of digital transformation in healthcare which are completely reshaping how we interact with health professionals, how our data is shared among providers and how decisions are made about our treatment plans and health outcomes.
Telehealth & Telemedicine
Up until 2020, it was an accepted part of Australian culture to receive healthcare in a face-to-face setting in the provider’s rooms or clinic. The COVID-19 pandemic is an unforeseen culture interloper. While our younger generations are ‘digital first’ by nature, COVID-19 is shifting this preference across the generations out of necessity.
According to findings by PwC there have been observed pockets of significant digital innovation in this space. These include:
- Austin Health in partnership with Arden Street Labs deploying a ‘digital first’ solution in which every COVID-19 test patient (positive or negative) can enrol in an online monitoring program with an app to detect and escalate clinical deterioration while they convalesce at home,
- University of Melbourne in partnership with Two Bulls recruited respiratory clinics and eligible primary care organisations to participate in a study which is based on a patient app targeted at those in isolation,
- South Australia has adopted Microsoft Teams across its health department in response to COVID-19.
- The Royal Prince Alfred Hospital in Sydney opened the first virtual ward in Australia.
Important to note however, we have yet to see these innovations translate to systemic change at the whole of state or national level.
Process Automation
Emerging digital technologies, such as robotic process automation and intelligent automation, hold great promise to deliver better quality care at a lower cost. Due to the COVID-19 pandemic, physicians experienced the rapid adoption of these new tools – and their benefits
According to a recent, US-Based Deloitte Insights report , when asked about opportunities for automation, physicians prioritise automating administrative tasks over patient interactions. Among activities presented in the survey, physicians say coding and completing prior authorisation requirements (typically performed by other staff) are most promising for automation, as are data entry requirements.
The healthcare segment for Robotic Process Automation (RPA) is expected to be one of the fastest-growing sectors over the coming years. This is not a surprise since healthcare systems contain multiple rule-based processes and generate a substantial amount of data.
Data & Analytics
The growth in the amount of data collected on our health, from our interaction with health services as well as our own devices and online activities, means providers have an increasingly accurate picture of where and when intervention may be needed.
As noted by Forbes , the pandemic has shown us that there is a willingness to share our personal data when the benefits to our health are clearly communicated. This has been proven by track-and-trace systems that have reliably kept infection levels in check in some regions (though less so in others).
When data is consolidated, automated and standardised, and supported by comprehensive governance frameworks there exists an opportunity to harness real-time insights to better inform decision making – whether this be operational, strategic or care-based. Using big data and advanced analytics, you can analyse real-time information to enable proactive patient care and ensure data-driven decision-making, improving the quality of care, while simultaneously lowering costs.
AI & The Future of Health
Healthcare leaders are making big bets on AI. According to findings in a new KPMG research report, healthcare business leaders express confidence in AI’s ability to help solve major industry problems, particularly those we are facing today – tracking the spread of COVID-19 and helping with vaccine development and distribution.
Healthcare business leaders say their organisations are prioritising their AI investments during the next two years on telemedicine (38%), robotic tasks (37%) and the delivery of patient care (36%), according to KPMG’s survey.
Additionally, AI has effectively played a role in acting as the digital front door for hospitals. Technology used for voice recognition or to uncover keywords in chatbots enabled calls and messages to be routed to the most appropriate source. Use of these technologies has more recently been important in vaccine management to improve communications and more proactively inform adversely impacted populations.